Abstract
Recurrent disease relapse and remission is a hallmark of indolent non-Hodgkin lymphoma (NHL). Remissions are often characterised by long periods of clinical inactivity without detectable disease. Furthermore, it is now standard practice to clinically monitor carefully selected asymptomatic patients with indolent lymphoma, often for years, reserving therapy for symptomatic disease progression, without adversely affecting the patient's prognosis. Identification and targeting of the putative cellular reservoir recurrently seeding disease relapse and progression in NHL has long tantalised researchers and would represent a significant advance in the field given the hypothetical prospect of deferring or preventing impending relapse.
The oncogene EZH2 is upregulated in the lymphoid germinal center and forms the enzymatic core of Polycomb Repressive Complex 2 (PRC2) alongside essential core components EED and SUZ12, writing all methylation of H3K27, with H3K27me3-mediated silencing of the B-cell terminal differentiation programme. The EZH2 small molecule enzymatic inhibitor Tazemetostat has been approved as monotherapy beyond second line for relapsed/refractory EZH2-mutant and wild-type follicular lymphoma, with responders benefiting for a modest median duration of 10.9 months (Morschauser et al., Lancet Oncology, 2020). The mechanism(s) for disease progression in patients have not yet been published.
Using TIG3-T human diploid fibroblasts as a model of cellular quiescence, we discover that a novel form of PRC2 predominates in non-dividing cells, which contains EZH1, EED, SUZ12 and the polycomb-like protein, PHF1, but crucially lacks EZH2. RNA-Seq and Western blot analysis revealed reciprocal expression patterns of EZH1 and EZH2 in serum-starved, quiescent (non-dividing) cells compared to asynchronous cycling cells.
Using EED immunoprecipitation with subsequent mass spectrometry, we demonstrated that EZH1 replaces EZH2 as the predominant H3K27 methyltransferase in quiescent cells. Quantitative ChIP-sequencing with exogenous reference genome spike-in (ChIP-Rx) confirms that EHZ1-PRC2 largely replaces EZH2-PRC2 at polycomb target genes. While the EZH2 enzymatic inhibitor GSK343 and the EED allosteric inhibitor A395 significantly reduced H3K27me2 and H3K27me3 in cycling cells, those markes are unchanged in quiescent cells. This alludes to a function of EZH1-PRC2 in quiescent cells that is independent of its function as a H3K27 methyltransferase, and therefore not targetable by PRC2 enzymatic inhibitors.
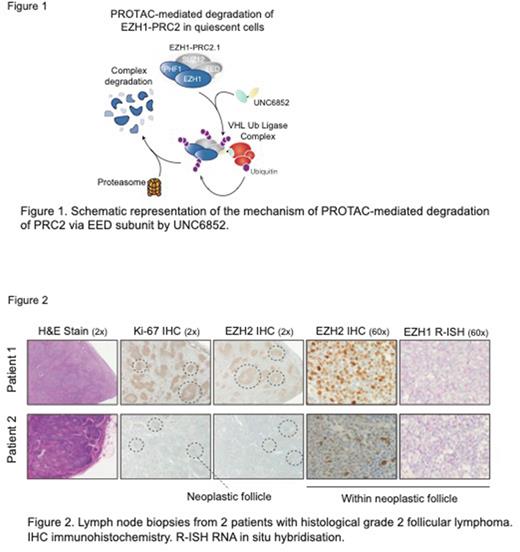
The EED PROTAC UNC6852 degrades EED (Figure 1), thereby destabilising both EZH1-PRC2 and EZH2-PRC2, as confirmed by Western blot and ChIP-Rx. Strikingly, this molecule resulted in a marked reduction of H3K27me2 and H3K27me3 in proliferating cells, but had no such effect in treated quiescent cells. Degradation of PRC2, however, did result in a modest reduction in protein levels and chromatin occupancy of the canonical PRC1 component CBX7, suggesting an interplay between EZH1-PRC2 occupancy and local cPRC1-mediated chromatin of compaction of Polycomb target genes.
EZH2 and Ki-67 immunohistochemistry and EZH1 RNA in situ hybridization (RNA-ISH) were performed on lymph node biopsy specimens from two well-matched patients with histological grade 2 follicular lymphoma (Figure 2). Patient 1 has multiply relapsed follicular lymphoma, rapidly requiring therapy following this biopsy. Patient 2 presented with a right inguinal mass and stage 3A disease, though did not require therapy for 14 years from the time of this biopsy. Interestingly, while both patients harbour abundant EZH1-positive cells (approximately 60% of cells within neoplastic follicle), only patient 1 whose tumour expressed abundant EZH2 and Ki-67 had clinically active disease requiring therapy. Although this requires validation in a larger series, these cases illustrate the presence of lymphoma cells in both patients likely to be refractory to PRC2 enzymatic inhibitors in vivo.
In summary, we propose that EZH1-PRC2 delineates a non-proliferating, PRC2 enzymatic inhibitor-resistant population of cells that could serve as a disease reservoir in indolent NHL. These cells are targetable by PROTAC-mediated EZH1-PRC2 degradation, with the resultant disruption reflecting the non-enzymatic roles of EZH1-PRC2. EZH1-PRC2 should be addressed as a therapeutic target to treat NHL in the future.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal